Sub-optimal disease control
Further understanding
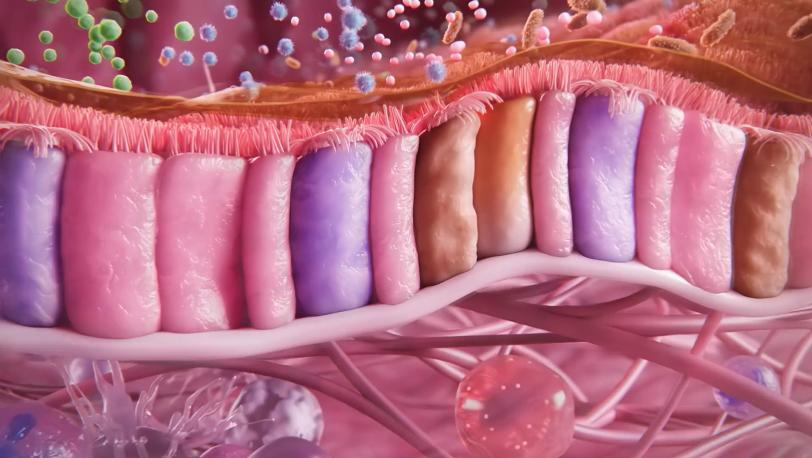
Much of respiratory disease pathogenesis can be understood by exploring the Type-2 and beyond Type-2 inflammatory cascades that start at the epithelium.3,4,6,7 Increased understanding of the epithelium should therefore inform scientific exchange, exploring ways to improve disease stability and achieve remission.8-10
Earlier monitoring
Earlier and more regular monitoring is crucial to manage the dynamic and complex nature of epithelial-driven disease and better patient outcomes.7,11,12
Professor of Pulmonary, Critical Care and Sleep Medicine, University of Washington
“My particular interests are the management of difficult-to-control asthma and the pathogenesis of airway hyperresponsiveness including exercise-induced bronchoconstriction.”
Professor of Pulmonary Medicine, University of Kiel and Director of the Department of Pneumology, LungenClinic Grosshansdorf
“My research encompasses several fields of respiratory medicine, including asthma, COPD and lung cancer, with the aim to investigate the mechanisms of airway inflammation, early determinants of lung health and the pathophysiological links between respiratory and cardiovascular disease.”
Consultant ENT Surgeon and Professor of Rhinology at King’s College
“My research focuses on improving outcomes of medical and surgical treatments for nasal conditions.”
Professor of Medicine and Associate Chief of Clinical Research and Practice Innovation, Northwestern University
“My primary research focus is in chronic rhinosinusitis and comorbid conditions. I have published more than 100 peer-reviewed articles in this field.”
Professor of Internal Medicine, Division of Pulmonary and Critical Care Medicine, University of Michigan Health System and Director of the Michigan Airways Program
“My research interests are related to large clinical trials in COPD, defining disease phenotypes, new screening methods and treatment interventions, as well as the impact of smoking and smoke exposure on lung health.”
Associate Professor of Internal Medicine, University of Naples Federico II
“My research area of interest is on the pathogenesis of bronchial asthma and allergic diseases, including the roles of eosinophils, basophils, mast cells, macrophages and specific cytokines in allergic disorders.”
Professor of Respiratory Medicine, University of Oxford
“My research focuses on identifying and validating biomarkers of eosinophilic, Type-2 airway inflammation in asthma and COPD.”
Associate Professor of Medicine, Harvard Medical School
“My primary research focus is on the causative mechanisms of AERD, severe asthma and nasal polyposis.”
Associate Professor of Internal Medicine, Humanitas University
“My main clinical interests focus on inflammatory airway diseases, immunological mechanisms of allergic diseases, asthma, rhinitis, chronic rhinosinusitis with nasal polyps, anaphylaxis and food allergy.”
Professor of Medicine, Department of Medicine, Laval University
“In the last three decades, I’ve been involved in research in asthma and respiratory allergy, as well as in education and knowledge translation in respiratory health.”
Associate Professor, Centre for Heart Lung Innovation, University of British Columbia
“I am currently investigating how repeated cycles of injury and repair of the airway epithelium contribute to the development of asthma.”
Assistant Professor in Medicine, Université de Sherbrooke
“EpiCentral is an important platform to tackle our rapidly evolving knowledge of the airway epithelium as the epicentre of asthma.”
Professor in the Department of Respiratory Diseases, University of Aix-Marseille
“My particular interest is in the bronchial epithelium and its relation to allergy and environment in chronic severe bronchial diseases.”
Assistant Professor in Asthma, Allergy and Clinical Immunology, Department of Medicine, University of Verona
“My research interests focus on immunological and allergic diseases, in particular severe asthma and rare dysimmune conditions with hyper-eosinophilia.”