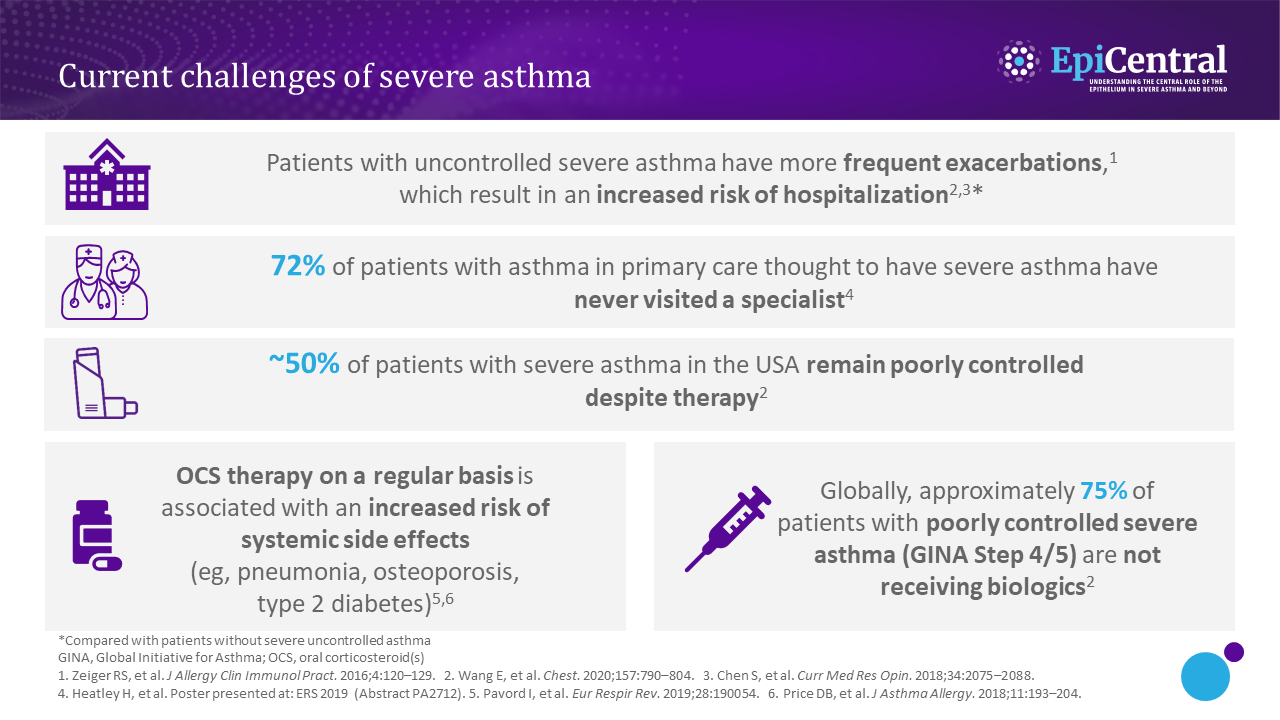
The long-term goals of severe asthma management include: achieving good symptom control, reducing the future risk of exacerbations, and minimizing lung function decline and airflow limitation.2 In many cases where patients have poor symptom control and/or exacerbations despite medium- or high-dose ICS and LABA therapy, their asthma may appear difficult to treat because of contributory factors, such as incorrect inhaler technique, poor adherence, smoking or comorbidities, or because of incorrect diagnosis.2 For these patients, GINA recommends assessment of these contributory factors and consideration of an add-on therapy.2 If problems persist, referral to a specialist center for phenotypic assessment and consideration for add-on biologic-targeted treatments are recommended.2
Confirming the diagnosis of asthma, assessing contributory factors, and optimizing treatment strategy are the key steps for consideration in the diagnosis and management of severe asthma.2
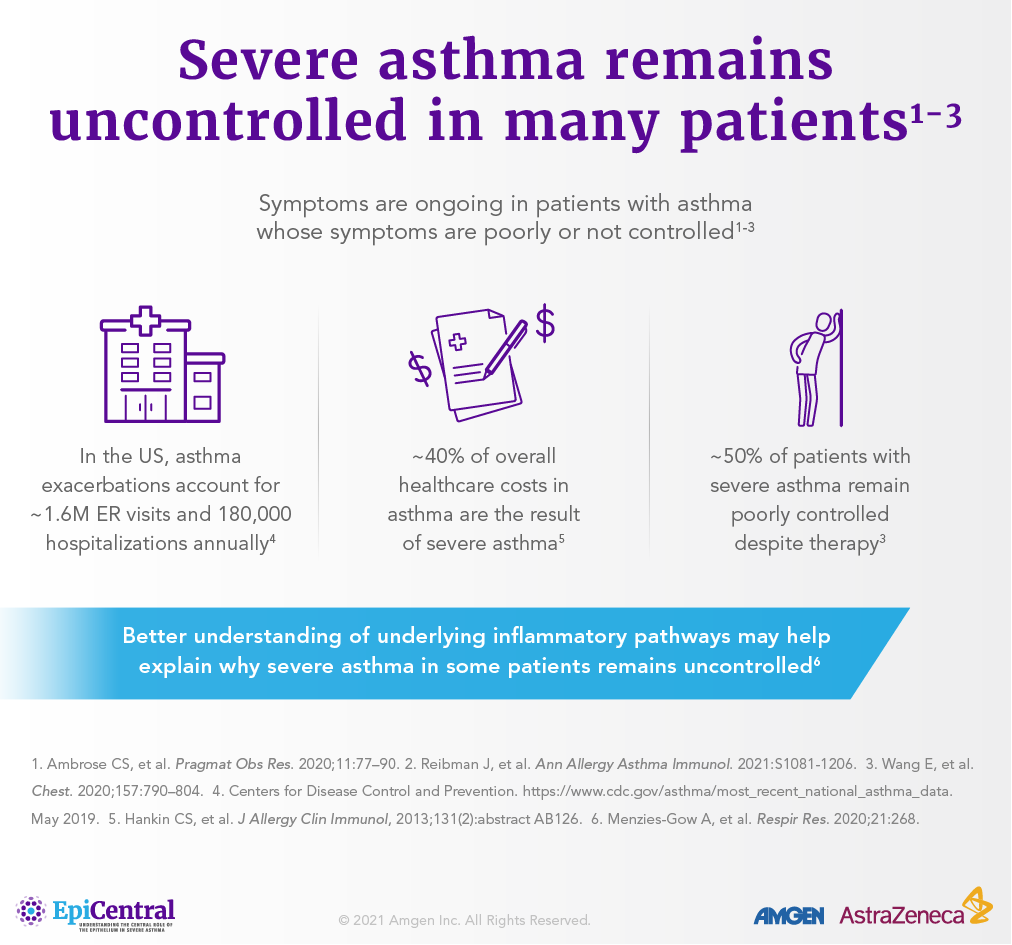
To date, there has been great progress in the diagnosis and management of severe asthma,5,6 with biologics representing a major advancement in the treatment landscape.7 However, many patients with severe asthma are poorly controlled.
A recent study found that approximately 50% of patients with severe asthma in the USA remained suboptimally controlled despite treatment with standard-of-care medications.8 This significant finding was described following a retrospective and prospective analysis of the International Severe Asthma Registry – a data set including 3286 US patients receiving GINA Step 5 treatment or with severe asthma remaining uncontrolled at GINA Step 4 (December 2014 to December 2017). Poorly controlled asthma was defined in this study according to Asthma Control Test (score 5–15) or Asthma Control Questionnaire (score >1.5) categorizations.8